TLDR: A drug that has been used for millennia suddenly needs to go through FDA approval; goes about as well as you’d expect.
I. Background
I wanted to start off with a short and succinct description of the mechanism of action of colchicine, something like, “Colchicine treats gout by inhibiting microtubule formation in neutrophils, disrupting the inflammatory response to uric acid crystal deposition.” Then I realized I haven’t spoken to someone not in medicine since May of this year, and figured I should probably translate this into Standard English.
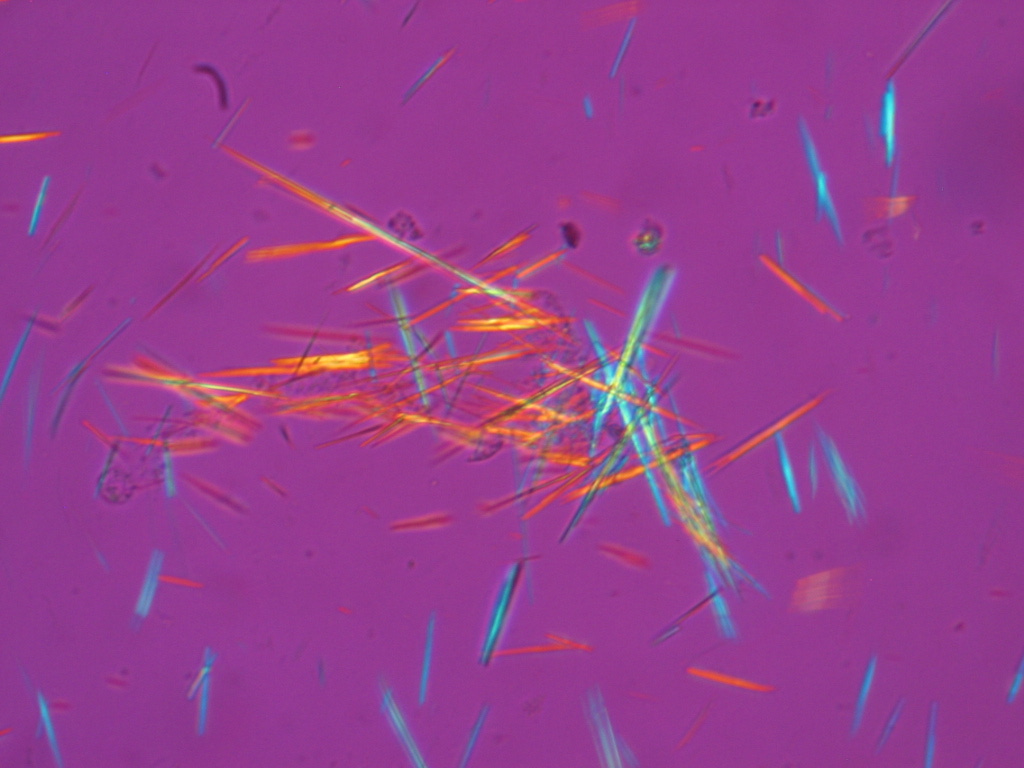
Gout is a type of joint pain, most commonly in the big toe, caused by uric acid crystal buildup. Uric acid is itself a byproduct of our body breaking down purines (the A and G bases found in DNA and RNA), which then get filtered through the kidneys from the blood and excreted in our urine.
Sometimes, either via cancer, drugs, or simply consuming too much alcohol and meat, we can get hyperuricemia, or an increased concentration of uric acid in our blood. Since our kidneys can only filter so much at once, the excess uric acid tends to form urate crystals in our joints. Since these crystals aren’t supposed to be there, they cause neutrophils to enter the joint space and eat them, which causes neutrophils to release the signaling proteins they have stored. These signaling proteins, in addition to calling for more neutrophils to join in on the fun, sensitize the nerve endings in the area to pain, eventually causing what we know as acute inflammation.
These gout attacks can be extremely painful. Some patients describe the pain as “burning,” “cooking,” and “fire in the joints.” The pain untreated can last five to seven days before subsiding.
Fortunately, treatment for gout is pretty simple: disrupt the inflammatory response, stop the pain. The three main ways of doing this are NSAIDs (ibuprofen), glucocorticoids (a class of steroids), and colchicine. I had heard about NSAIDs and steroids before medical school, but colchicine was new.
Colchicine works by inhibiting microtubule formation in neutrophils. Microtubules are most famously known for “those things that pull apart chromosomes in mitosis,“ but in neutrophils they are used regularly to help the cell move around the body. Disrupting microtubule formation prevents neutrophils from getting into the joint space, which stops the positive-inflammatory feedback loop seen in gout.
Colchicine’s medical use dates back to 1550 BC, where Egyptians would use the corms of the *Colchium autumnale* plant as a herbal remedy for gout. Colchicine was isolated from the plant in the 1800’s, and has since largely been prescribed by doctors in its pure form since then.
Ib. Now, This
In 2006, the Food and Drug Administration (FDA) launched the Unapproved Drug Initiative, which forced manufacturers to either run their unapproved drugs through FDA approval or take them off the market. Physicians had been using colchicine for literally hundreds of years before this, but there was no clinical trial at the time that “proved” (according to the FDA’s approval process) that colchicine was beneficial for gout.
Of the 21 companies made colchicine at the time, only one, URL Pharma, applied for FDA approval. They jumped through the regulatory hoops, and in 2009, received regulatory approval of Colcrys (colchicine’s patented new brand name) for gout.
According to the Waxman-Hatch Act, this act of regulatory approval granted them three years of market exclusivity to sell their drug in the United States.
*This absolutely was not abused at all. URL Pharma was satisfied to take the business from their competitors, didn’t raise the price at all, and was happy to contribute to the advancement of science and betterment of patient care.*
Or at least, that’s what probably happened in another universe. What URL Pharma did in our universe was jack up the price. What originally was $0.10/pill immediately became $5/pill with FDA approval, a twenty-fold increase.
Now, I can’t really blame URL Pharma here. With exclusivity rights over a time-tested drug, it’s practically hard-coded in their incentive structure to maximize their profit by charging as much as they felt Medicare would be willing to pay.
And at least for gout, it wasn’t so bad. Colchicine is used for gout flares, and since acute gout patients have one-to-two flares a year, it would cost… $20-$40/year? That does sound a bit pricy, but not exorbitantly so, and definitely something insurance should be willing to cover to save their patients two weeks of hellish pain. Furthermore, if a patient didn’t want to deal with recurring gout attacks, or had to pay out of pocket, they would always be able to take the alternative option of lifestyle/diet modifications. There were options available.
It wasn’t as if there was a unique sub-population that needed colchicine daily, and thus would be drastically impacted by this sharp rise in price… right?
Ic. From Bad, To Worse
In addition to gout, colchicine is the *only* treatment for Familial Mediterranean Fever (FMF), an autosomal recessive auto-inflammatory disease. Most common in mediterranean populations (who knew!), this disease causes patients to have recurring fevers lasting hours to days, in addition to abdominal, joint, and chest pain. Symptoms start to occur for 90% of patients before the age of 18, and requires lifelong colchicine to keep under control.
Colchicine’s jump in price was devastating to this population. Whereas patients with gout are often older and better-insured, FMF patients are often young and have to pay out-of-pocket. What once cost ~$150/year to keep under control ($0.40/day for four pills) became $7,300/year.
Furthermore, FDA-approval for Colcrys for FMF (which came soon after the original “for gout” approval) made it fall under the Orphan Drug Act, which granted seven years of market exclusivity to URL Pharma. Uninsured FMF patients were practically forced to rely on foreign sources of colchicine until they either got insurance or prices reached a level they could afford.
Id. Time Passes
This state of affairs persisted until 2014, when the FDA approved another manufacturer to produce generic colchicine. Takeda Pharma (who in the meantime purchased URL Pharma for a cool $800 million) in response sued the FDA for breaking their exclusivity agreement, which didn’t work, and in 2015 the FDA allowed manufacturers to make and sell generic colchicine again.
In the meantime, newer drugs have been developed so FMF patients are no longer solely reliant on colchicine to survive.
Ie. Why Care?
I like the story of colchicine because it is a specific example of systemic incentive failure in America. Somewhere along the way, from drug discovery, to drug policy, to drug ownership, profit got decoupled from providing optimal patient care. I don’t know if anyone has died due to failure to afford colchicine, but it abundantly clear the price hike caused unnecessary suffering for many patients.
I think the way to ”fixing our healthcare system” is by paying attention to well-documented stories like these, pinpointing exactly what went wrong, and fixing the incentive structures so they don’t happen again.



